Knee pain (gonalgia) occurs suddenly or gradually, either at rest, with movements or loads. Sometimes they are limited to a specific area, other times they affect the entire joint. Knee pain is often accompanied by other symptoms (e.g. redness or swelling). Read here what might be behind the pain and how it can be relieved.
Description
Without our knees, many everyday things would not be possible, such as walking or squatting. They usually do their job more or less inconspicuously for many years. But for many, one day, knee pain draws attention to this important support of our body.
Knee pain (gonalgia) occurs in the left and right knee, on one or both sides. Sometimes they are more likely to be felt in the front, back, inner or outer part of the knee, in other cases the entire joint is affected and the pain cannot be localized exactly.
Sometimes knee problems appear suddenly, in other cases they gradually increase. Depending on the cause, knee pain can be a temporary (treatable) health problem or a long-term problem.
In some sufferers, the knee pain is so severe that it is almost impossible to walk, stand or even sit for long periods of time. In such cases, coming to terms with such constant knee pain is a longer process that may require a lot of patience.
Not all damage to the knee manifests itself as classic joint pain . Sometimes pain radiating from the knee is felt elsewhere (such as the surrounding muscles). Conversely, supposed knee pain may have its cause in other parts of the body.
For example, injuries to the hip joint or spine sometimes radiate downwards, causing knee pain.
It is therefore very important to understand the basic structure and function of the knee and to find out the cause even if knee pain is unclear.
This is how the knee is constructed
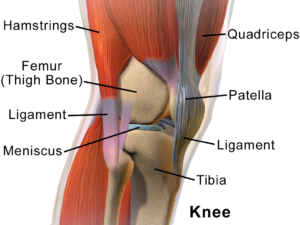
The knee joint is the largest joint in the human body and, strictly speaking, consists of two individual joints:
- The large, load-bearing joint between the thigh bone and shin bone.
- The joint between the kneecap ( patella ) and the thigh bone that is decisive for force deflection
The knee works mechanically like a hinge limited on one side. However, due to its sophisticated internal structure, it also offers a certain amount of leeway for slight twisting around the longitudinal axis.
The joint is sealed off from the outside by a cover of connective tissue (connective tissue capsule). Doctors therefore differentiate between damage or injuries inside (intra-articular) and outside of the joint (extra-articular).
In everyday life, the knee joint is sometimes exposed to high loads, for example when walking, running and jumping.
In order to cope with these loads, the knee joint is equipped with numerous structures that stabilize it, balance out and cushion forces.
Muscles, ligaments and tendons provide stability
Muscles and ligaments ensure the stability of the knee joint while maintaining mobility.
The so-called cruciate ligaments (one at the front and one at the back) and lateral ligaments (outside and inside) connect the upper and lower leg bones tightly with one another. They ensure that the thighs and lower legs remain in position with respect to each other and do not shift against each other.
Muscle power acts on the joint at the front via the strong patellar tendon and the kneecap. Smaller tendons from the hamstring muscles attach to the shinbone behind the knee. Smaller muscles work in the opposite direction: they pull from the posterior tibia to the femur.
menisci and bursa
Inside the knee, on top of the tibia bone, are two crescent-shaped cartilage disks called menisci . As a buffer, they absorb shock and pressure loads in the knee and distribute them evenly in the joint. In addition, they ensure that nutrient-rich joint fluid (synovial fluid) is evenly distributed over the articular cartilage.
There are also bursae in the knee. These fluid-filled connective tissue cushions sit in places where there is particularly high pressure and friction.
What are the causes?
Malfunctions, damage, wear and tear, inflammation or injuries to one or more components of the knee repeatedly lead to knee pain.
They are often caused by injuries in sports. Sports with abrupt stop movements and changes of direction are particularly risky, as are those in which the knee is bent and rotated under high loads. These include, for example, football, handball, hockey and alpine skiing.
Swimming also causes knee pain in some cases. This is how the so-called “swimmer’s knee” develops, for example when swimming the breaststroke, through repeated rotary movements in the knee joint. Fins add to this stress. Turning around in the pool for competitive swimmers also puts a strain on the knees and occasionally causes knee pain.
Strength sports also often lead to painful bruises, ligament strains and damage to the meniscus or cruciate ligament .
But knee damage and pain do not only occur during sports. Overloading and incorrect straining of the joint at work or in everyday life can also lead to this. For example, in parquet or tile layers – jobs where a lot of work is done kneeling on the floor and where arthrosis often occurs as a result.
Sometimes gonalgia also occurs when a knee joint is not used enough and the associated muscles are untrained.
In addition, wear and tear, metabolic disorders, autoimmune diseases and infections may also be possible causes.
Depending on where the knee pain originates from, possible causes can be narrowed down in some cases. Often, however, several parts of the knee are affected at the same time, which can make it difficult to determine the origin of the pain. This is mainly the case with injuries, but also with larger inflammations, bruises or the like.
Here you will find some causes of knee pain depending on the location:
1. Front knee pain
Common possible causes of pain in the front part of the knee are:
- patellar dislocation
If the kneecap (patella) jumps out of the sliding bed on the lower thigh, in which it normally runs, this is referred to as a patellar luxation ( luxation = dislocation). Most of the time, the knee brace jumps outwards.
Causes are:
- Traumatic: Force impact on the kneecap in a specific direction. In rare cases, patellar luxation occurs as a side effect of capsular ligament injuries of the knee due to direct trauma
- Atraumatic: Favored by factors such as misalignment of the axis, congenital malformations of the kneecap or plain bearings, or congenital or acquired anomalies of ligaments (“ligament laxity”) or muscles. Often due to sudden bending after a fall or twisting of the joint, then often recurring
- Congenital dislocation: For example, in nail-patella syndrome
- Permanent or long-lasting (chronic) dislocation: After recurring dislocations in childhood, mostly caused by very loose ligaments.
- Starting from the nerves (neurogenic): Cramping of certain muscles due to a “misdirection” by the nervous system may also lead to a patellar luxation
patella fracture
A patella fracture is a fracture of the kneecap bone. This is usually caused by violence, often from the front, for example in a car accident, when the knee hits the dashboard. Under certain circumstances, situations can also arise during sport that lead to a patella fracture .
The patella fracture is most common transverse, but also longitudinal or oblique. A distinction is also made between comminuted fractures (fractures in which several fragments are formed), bony avulsions and blasting off of bone and cartilage material.
In most cases, the knee can no longer be fully extended. In addition, there is often bruising and swelling in the joint (hemarthrosis).
In some people, the individual bone cores of the kneecap do not grow together, they then have a divided kneecap from birth (patella partita).
2. Inner knee pain (medial)
If the pain tends to originate from the inside of the knee (medially), the following causes can be considered:
- internal ligament tear
A medial ligament tear is a tear in the medial ligament of the knee, usually caused by sports injuries. It occurs either alone or in connection with an anterior cruciate ligament tear and a (inner = “medial”) meniscus tear . If all three occur at the same time, one speaks of an “unhappy triad” or an “unhappy triad”.
The cause is usually an outward rotation of the lower leg while the leg is stretched.
There is sudden or acute pain and swelling on the inside of the knee. If other structures are injured (e.g. in the “unhappy triad”), the joint may also become unstable.
- medial meniscus tear
Meniscus tears are often caused by the combination of flexion and rotation in the knee joint. Natural wear and tear (degeneration) is also a possible cause. The meniscus partially or completely tears off the shin roof.
Acute and sometimes severe pain often occurs first. In addition, there is often a bloody joint effusion. Later, patients may develop pain, which is felt primarily when the knee is bent and rotated at the same time (for example, while sitting cross-legged).
If an injury causes part of the meniscus to move into the joint space, the knee joint may no longer function properly. It can then no longer be fully stretched or, in some cases, is even completely blocked.
Tear injuries particularly often affect the meniscus on the inside of the joint (inner meniscus).
- Pes anserinus syndrome
The so-called pes-anserinus syndrome is caused by inflammation of the tendons in the hip or thigh muscles (sartorius, gracilis, semitendinosus muscles) or the bursa between them (pes-anserinus bursitis).
The cause is usually overexertion from sport, injuries or an imbalance between parts of the thigh muscles.
The pain often manifests itself on the inside of the knee joint or the upper part of the shin, especially when running, jumping or climbing stairs.
- Plica Syndrome
The irritation of a fold (plica) of the mucous membrane of the knee joint causes inflammation and pain, usually on the inside (medial) of the kneecap, especially under load or after an injury.
There may also be swelling, and the knee may no longer be able to stretch fully, so it feels blocked. Some patients also complain of stiffness after sitting for a long time.
3. Outer knee pain (lateral)
The following causes are common for pain on the outside of the knee (lateral):
- Runner’s knee (iliotibial band syndrome)
Runner ‘s knee or iliotibial band syndrome (ITBS) is a painful irritation of the fibrous cord that pulls externally from the thigh to the shin, preventing the thigh from moving outward relative to the lower leg. Runner’s knee usually manifests itself as a pressure-pain sensitivity on the outer knee or just below.
The cause is usually an overload of the local ligament apparatus. This is common in high-intensity runners and cyclists. Uncorrected “bow legs”, different leg lengths, inflammation of the bursa, incorrect running shoes or technique can also trigger an iliotibial band syndrome.
- External ligament tear on the knee
This is an injury to the outer knee ligament . The cause is usually a load on the knee while it is twisted outwards or bent away. Other knee ligaments (cruciate ligament or medial ligament) are often injured as well.
There is massive pain, especially under stress, the knee swells and there may also be a bruise.
Overall, tearing of the outer ligament of the knee is less common than tearing of the inner ligament.
- lateral meniscus tear
The outer meniscus tear is significantly rarer overall than the inner meniscus tear (see there). However, it is also usually caused by wear and tear (degeneration) or injury caused by twisting and bending the knee at the same time.
Here, too, there is acute pain, joint effusion and limited stretchability of the knee.
4. Back knee pain
If the pain originates in the back of the knee – i.e. around the back of the knee – the main possible causes are as follows:
- Muscle and tendon injuries
Injuries to the hamstrings are common during sports, especially sprinting. Tendon injuries to the “semitendinosus muscle” (musculus semitendinosus) are usually noticeable through pain in the rear, outer knee (posterolateral).
Favorable factors include insufficient warm-up, overexertion or incorrect running technique.
In rare cases, nervous symptoms occur. This happens, for example, when swelling from a bruise presses on a nerve.
Injuries to the “twin calf muscle” (musculus gastrocnemius) are particularly noticeable when bending the knee or calf raises. In some cases they occur alone, but in others they also occur in connection with other muscle damage – especially in muscles of the thigh.
The popliteal tendon is usually triggered by an injury while the knee is in extension or overuse while stabilizing the joint laterally to the rear (posterolateral).
Pain on the rear, outer knee – often with bruising in the joint – may indicate an injury to the popliteal tendon. Also, if you experience pain at the beginning of the swing phase of the lower leg when walking or when loading the knee in a 15-30° flexion, an injury to this tendon may be the cause.
- cruciate ligament tear
There are two cruciate ligaments in the knee, one anterior and one posterior. They prevent the thigh bone from shifting against the lower leg bone under load.
Back knee pain is more likely to indicate a tear in the posterior cruciate ligament. This occurs, for example, in car accidents when force is applied to the stretched knee from the front. If this movement or force is not sufficiently absorbed by the surrounding muscles because it is too sudden or too strong, a cruciate ligament tears in some cases.
The posterior cruciate ligament alone is rarely torn, usually the anterior and/or the outer ligament as well. Overall, tears in the posterior cruciate ligament are less common than those in the anterior cruciate ligament.
Other, less common causes
There are a few other causes that, in rare cases, lead to back knee pain. These include injury or irritation of the fibula nerve, which is part of the sciatic nerve. Nerve-related pain often feels burning.
Vascular diseases such as an “enlargement of the arteries” ( aneurysm ) or a “blood clot” ( thrombosis ) also lead in some cases to knee pain in the rear area.
Bone injuries or fractures, more rarely degenerative bone diseases or bone tumors are also expressed in rare cases by pain on the back of the knee.
Knee pain regardless of location
Not only where, but also when the pain occurs, in some cases there are indications of the possible cause:
- Start-up pain (break-in pain): This is what knee pain is called, which is noticeable at the beginning of a movement in the joint and decreases with further movement. The cause is often wear and tear ( arthrosis ) of the knee joint (gonarthrosis). This is often noticeable when climbing stairs, getting up or walking downhill.
- Movement pain: If the knee pains more or less persistently during movements, this is often due to a recent injury (e.g. tendons, ligaments, bursae, menisci).
- Stress pain: If the knee pain only occurs when the joint is under stress, for example when walking, this may indicate a meniscus injury. If the knees hurt, especially when they are strained when climbing stairs, the pes anserinus syndrome (see above) is one of the possible causes.
- Pain at rest: If the knee pain (also) occurs at rest, i.e. at night or generally when lying down or after sitting for a long time, rheumatoid arthritis may be the reason. Degenerative diseases such as arthrosis or other diseases sometimes make themselves felt through pain at rest or at night.
However, sometimes knee pain cannot be attributed to a specific part of the knee, activities or periods of time during which it is felt:
injuries
Injuries can occur in almost any part of the knee. The pain then occurs at the site of the injury, possibly also in the immediate vicinity:
- Bruises are a common cause of knee pain. A bruise usually occurs outside of the joint capsule as a result of an impact, blow or fall. The skin in the affected area turns bluish-red.
- Strains are overstretching of muscles, ligaments, the capsule or the tendons around the joint. They become noticeable through bruising and pain. In addition, the affected knee feels less stable for the patient for a time.
- Muscle and tendon tears in the knee joint – in otherwise healthy people – usually only occur when excessive force is applied and are therefore particularly common in athletes. Collateral ligament, tendon attachment or patellar tendon tears are usually accompanied by bruising. Often the joint cannot be moved or loaded as usual and feels unstable.
- Broken bones are also possible causes of knee pain. The injury affects either the head of the tibia bone, the so-called condyles of the thigh bone, or the kneecap. A bone injury sometimes also occurs with a cruciate ligament rupture, when a piece of the bony anchorage tears out.
- Open wounds such as abrasions or cuts are mostly harmless knee injuries. If the injuries are deeper and may have damaged the joint capsule, there is an increased risk of infection. If the doctor suspects such an injury to the joint capsule in a patient, an operation is required as soon as possible.
inflammation
Sometimes the pain in the knee is caused by inflammation of the joint. In some cases they are triggered by infections, but there are also rheumatic diseases and certain metabolic disorders that attack the inside of the knee joint:
- In chronic rheumatoid arthritis (chronic polyarthritis), which usually occurs in phases, immune cells attack the synovial membrane. This becomes inflamed and produces inflammatory substances that destroy the connective tissue and articular cartilage. Long-lasting (chronic) knee pain occurs.
- Bechterew’s disease (ankylosing spondylitis) also belongs to the group of rheumatoid diseases. In addition to inflammation, there is increasing curvature of the spine. Patients usually try to compensate for this curvature by bending their hips and knees. Knee pain is one of the possible consequences.
- Arthrosis (on the knee also knee joint arthrosis or gonarthrosis) refers to the wear and tear of the joint. The cartilage covering the joints wears away until finally the bones rub directly against each other. Depending on where the cartilage is damaged, pain is more likely to be internal or external. A “weather sensitivity” often shows up in colder weather.
- In gout , the uric acid content in the blood is greatly increased. The excess uric acid is then deposited in salt crystals in the joints (such as the knee joint), irritating and damaging the synovial membrane and cartilage. Gout in the knee often manifests itself in spurts with very painful swelling and overheating.
- In pseudogout (chondrocalcinosis) , calcium salt crystals form and are deposited in the cartilage. This often has consequences similar to the accumulation of uric acid crystals in gout.
- Reactive arthritis (formerly: Morbus Reiter or Reiter’s syndrome) is another representative of the rheumatoid group. It is an inflammation that may occur after certain bacterial infections of the gut, urinary tract, or genitals. In some cases, the disease also causes knee pain.
- Rheumatic fever is caused by certain bacteria , a type of streptococci. It affects the knee joints and other joints, as well as the heart , kidneys, and nervous system.
- Injuries that also damage the joint capsule often result in bacterial infections that lead to joint inflammation (arthritis). If the knee is affected, knee pain may also occur.
- Tick-borne Lyme disease is often asymptomatic, but in some cases leads to joint inflammation. The knee joints are often affected, and in some cases other large joints, such as the ankle , are also affected . In addition, there are usually symptoms such as erythema and, in some cases, nerve pain .
- Systemic lupus erythematosus is an autoimmune disease in which the immune system attacks the body’s own cells . So-called immune complexes are formed from antibodies and the attacked cell structures. Under certain circumstances, they are deposited in the knee, which then leads to painful inflammation of the inner lining of the joint.
- Psoriatic arthritis also belongs to the rheumatoid group. It is a chronic joint inflammation that occurs in connection with psoriasis . If the knee joint is affected, the resulting knee pain gets progressively worse. But there are also longer symptom-free phases.
- Tendon and bursa inflammations are caused by injuries, infections or overexertion.
Other causes
There are also a few other possible causes of knee pain that cannot be assigned to any of the previous categories. They are partly innate, but partly also only develop in the course of life:
- Osteochondrosis is a disorder of bone formation in children. They occur during the growth phase and are noticeable, among other things, through knee pain.
- Osteonecrosis refers to the death of a section of bone (e.g. Osgood-Schlatter disease, see above). It is either caused by bacteria (septic) or by a nutritional disorder of the bone (aseptic). Injuries also lead to osteonecrosis in some cases when bone nutrition is disrupted.
- Functional disorders (congenital or acquired) in the hip joint lead in some cases to pain in the knee. Either the pain actually originates in the hip and only radiates to the knee. Or the disturbance of the hip function impairs the movement chain and thus causes incorrect loading of the knee, which results in pain.
- Haemophilia is an inherited disease in which blood does not clot properly. This can lead to sudden joint bleeding. The resulting increase in pressure inside the joint can lead to pain in the knee.
- Malignant, but also benign tumors are in some cases the cause of knee pain. They may occur in bones, fat or connective tissue, in blood vessels or in the inner lining of a joint.
- Occasionally there is a psychosomatic cause behind chronic knee pain .
- So-called “growing pains” are often pulling pains in the limbs, often at night, especially in children. The cause is so far unclear. In fact, growth is painless. Therefore, the doctor first rules out all other possible causes before assuming a “growing pain”.
What to do with knee pain?
Many sufferers wonder what helps against knee pain. Depending on the cause of the pain, there are different ways to relieve it:
In the case of acute injuries to the knee joint, the first thing to do is to relieve the joint, relieve the pain and counteract swelling. Use the so- called LUCKY rule for orientation : pause , ice , compression , elevation .
Cooling causes blood vessels to constrict and bruises to stop growing. Elevation also reduces blood flow to the injured area. The knee can also be stabilized with a tight bandage (compression).
Quarry poultices have also often proven themselves as an anti-inflammatory and pain-relieving (because cooling) home remedy.
If the knee pain is related to a rheumatic disease, warming is often more pleasant than cooling.
If the knee pain is due to irritation or inflammation of the tissue or a bruise, sports ointments and taking enzyme tablets often provide relief. An enzyme from the pineapple fruit , for example, has an anti-inflammatory and decongestant effect.
If necessary, painkillers are also available for knee pain. In the pharmacy you can get non-prescription preparations from the group of non -steroidal anti -inflammatory drugs ( NSAIDs ) such as acetylsalicylic acid (ASA), ibuprofen, naproxen or diclofenac . They have a pain-relieving and anti-inflammatory effect.
Consult a doctor or pharmacist for advice on the choice of painkiller, dosage and use.
treatment by the doctor
Effective pain management is very important in the treatment of knee pain. The doctor recommends or prescribes a suitable painkiller for the patient. In doing so, he takes into account any contraindications (contraindications) – i.e. circumstances that speak against the use of a specific drug.
For example, people with a stomach ulcer are better off not taking painkillers from the NSAID group.
Practically all more complex knee diseases and the associated knee pain belong in the hands of specialized doctors – for example orthopedists and radiologists for the precise diagnosis and surgeons for an operation that may be required.
The treatment of knee pain depends on the cause. For example, if the pain is related to an open injury, this is surgically cleaned and, if necessary, closed. Due to the high risk of infection for the knee joint, special care is important.
In the event of blood or irritation in the knee, a puncture may provide relief. The accumulated liquid is drawn off with a hollow needle.
With some injuries, the pain in the knee can be relieved with bandages or special splints. At the same time, the range of motion of the joint is restricted. This gives the damaged structures the opportunity to heal in peace.
If necessary, the doctor also prescribes physical and physiotherapeutic treatments for knee pain. These include, among other things, ultrasound or electrical stimulation therapy, medicinal baths, manual therapeutic grips and physiotherapy exercises.
If other diseases, such as rheumatism or psoriatic arthritis, are the cause of knee pain, these are treated separately.
When is it better to go to the doctor?
Obvious reasons for knee pain such as superficial abrasions, minor bruises or strains on the knee joint can usually be treated by yourself and without medical help. For deeper wounds , however, a doctor’s visit is urgently needed. This is especially true if the joint capsule may have been injured.
Then there is the danger that germs have unhindered access to the interior of the joint. If such infections and serious joint injuries are not treated, in the worst case the joint function is partially or completely lost – the joint stiffens.
See a doctor even if you have bone, ligament, or cartilage damage in your knee .
Ideally, you should also have knee pain checked by a doctor in the following cases:
- The knee pain is very strong .
- The cause of the pain is unclear .
- The symptoms last for several days (despite rest, heat or cold treatment, painkillers, home remedies, etc.) or occur in phases .
- Knee pain is accompanied by other symptoms such as redness, swelling and overheating of the joint, bruising, restricted mobility of the joint or fever.
investigation
The doctor first conducts a detailed discussion with the patient to collect the medical history (anamnesis). Among other things, he asks how long the pain has existed and whether there is a probable trigger (such as an accident, physical exertion).
The exact location of the knee pain (e.g. inside, outside), its progression and any underlying diseases (such as rheumatic diseases or metabolic disorders) are also important for the diagnosis.
The doctor also asks whether any therapy attempts (such as bandages, cooling or pain ointments) have already been made and how well they worked.
Physical examination
During the physical examination, the doctor tests how far the affected person’s knee joint can be bent under their own power (active flexion) and how far it can be bent painlessly with help (passive flexion). If necessary, this test also provides information on how severe the knee pain is.
The doctor also scans the tendons and ligaments in the knee area for any abnormalities, such as palpable injuries or pain when pressure is applied.
An important function test for the cruciate ligaments is the drawer test: If the head of the tibia can be pulled forward in relation to the femur, the anterior cruciate ligament is unstable (torn). If, on the other hand, it is possible to push the tibial plateau backwards in relation to the thigh, the posterior cruciate ligament is damaged.
The doctor may also ask the patient to walk up and down a few steps to assess the gait. For example, limitations in mobility and protective posture become visible.
imaging
Imaging examinations are often necessary to clarify knee pain:
- An ultrasound examination can be used to detect, for example, major damage to tendons and ligaments or a knee joint effusion.
- Using an X-ray examination , the doctor discovers broken bones or deviations in the joint position, and the thickness of the joint cartilage can also be assessed in this way. Bone deformations typical of arthrosis or inflammatory joint diseases are also visible on the X-ray image.
- Computed tomography (CT) uses an X-ray beam orbiting the patient to create detailed tomographic images of the knee joint. Many changes inside the joint can be recognized in this way.
- Another tomography method, magnetic resonance imaging (magnetic resonance imaging or MRI), is particularly well suited to detecting hidden damage to ligaments, tendons or menisci inside the knee joint. No X-rays are used in the examination, but rather strong magnetic fields.
- A scintigraphy is a nuclear medicine examination. The doctor makes the metabolic activity of different tissues visible with the help of radioactively marked substances. This makes it possible to identify inflammation or dead bone tissue.
Further investigations
The doctor may order further tests:
- In some cases, damage to the knee joint can be assessed more precisely with the help of a joint reflection (arthroscopy). To do this, the doctor inserts an instrument equipped with a camera (endoscope) into the joint through a small skin incision. Surgical interventions on the joint can also be carried out with the help of such an endoscope.
- An angiography is an X-ray examination of the blood vessels . The patient is injected with a contrast medium that makes the vessels clearly visible on the X-ray image. Circulatory disorders or dead bone parts (osteonecrosis) can be proven to be the cause of knee pain.
- A blood test may give indications of infections, autoimmune or rheumatic diseases. Metabolic diseases such as gout can also be detected using blood values.
- Urine or stool tests are carried out in particular to detect germs (such as bacteria), since some pathogens can lead to an inflammatory reaction within the joint.
- In some cases, an examination of the synovial fluid is useful. It is checked whether the liquid has a pathologically altered composition or whether it contains bacteria or antibodies.
- If rheumatic fever is suspected, a throat swab is taken and analyzed in the laboratory.
- Examinations of the skin may provide indications of possible psoriatic arthritis.
- If a benign or malignant tumor is suspected, tissue removal ( biopsy ) may be required.
Prevent
Suitable footwear or special knee pads offer a certain degree of protection against knee injuries.
Knee bandages or “taping” the knee may also help. This is advisable for sensitive people who, for example, have had knee problems before, as it helps to stabilize the knee. However, it is better to only use these measures when they are absolutely necessary – for example during training, games or competitions.
Regular and balanced training of the entire musculature around the knee joint is more important for the prevention of knee injuries. Strong muscles stabilize the knee joint and often effectively prevent knee pain.
